MPFL Reconstruction Surgery
Medial patellofemoral ligament (MPFL) surgery is a surgical procedure designed to restore stability to knees affected by patellar instability or recurrent dislocation. This article provides a comprehensive overview of MPFL reconstruction surgery, drawing from my personal experience as an orthopedic surgeon specializing in knee injuries and research I have personally been involved with.
MPFL Reconstruction Surgery: Restoring Knee Stability
The MPFL is a critical stabilizer of the kneecap (patella), anchoring it to the femur and preventing it from sliding out of place. When this ligament is injured, patients may experience repeated knee (patella) dislocations, pain, cartilage injury, and a loss of confidence in their knee’s stability. MPFL reconstruction surgery is a proven solution for restoring function and preventing further injury, especially in cases where conservative treatments have failed.
Understanding the MPFL
Anatomy of the Knee
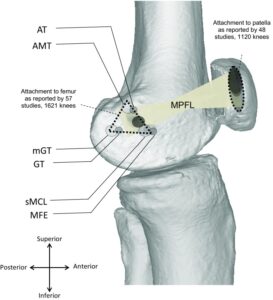
The knee joint is formed by the patella (kneecap), femur (thigh bone), and tibia (shin bone), stabilized by several ligaments. Connecting the inner edge of the kneecap to the thigh bone, the MPFL works to stabilize the kneecap during movement.
Role in Stability
The MPFL is the primary restraint against the patella dislocating laterally (outward). When functioning properly, it works as a leash to keep the patella within its groove on the femur.
How MPFL Injuries Occur
MPFL injuries typically result from direct trauma, sports injuries, or twisting motions that force the kneecap out of its groove. Anatomical predispositions, such as a high-riding patella (patella alta), ligamentous laxity, or a shallow trochlear groove, can increase the risk of injury.
Conditions Treated with MPFL Reconstruction Surgery
- Patellar Instability: Repeated episodes where the kneecap slips or subluxes out of place..
- Recurrent Knee Dislocations: More than one dislocation, often after an initial traumatic event.
Common Symptoms
Patients with MPFL injuries may experience:
- Persistent pain around the kneecap
- A sensation of the knee “giving way” or instability
- Frequent dislocations or partial dislocations (subluxations)
- Swelling and/or stiffness after prolonged sitting
- Loss of confidence in the knee’s ability to support weight, especially when going down the stairs.
When to Consider MPFL Surgery
MPFL reconstruction surgery is recommended when patients experience:
- Recurrent patellar dislocations
- Persistent sensation of instability
- Failure of a trial of conservative treatment to restore function and confidence
Diagnosing Patellar Instability
Clinical Evaluation
A thorough history and physical examination are essential. The surgeon assesses knee alignment, ligament laxity, and patellar tracking.
Imaging Techniques:
Getting good images is important for surgeons to understand what exactly is happening in the knee. Expect your doctor or surgeon to require the use of one or more of the following imaging techniques:
- X-rays: Evaluate bone alignment and patella height.
- MRI: Visualizes soft tissue injuries, including the MPFL and cartilage.
- CT Scans: Provide detailed images of bony anatomy and alignment.
Preparing for MPFL Surgery
- Initial Consultation: Comprehensive evaluation to confirm diagnosis and assess risk factors and outcomes.
- Pre-Operative Tests: Imaging studies as needed.
- Discussion: Review of surgical risks, benefits, and realistic expectations. Patients are encouraged to ask questions and understand the rehabilitation process and timeline.
What to Ask Your Surgeon
Before having surgery to repair your MPFL, make sure to ask your surgeon these questions:
- What is my specific diagnosis?
- What are my treatment options, both surgical and non-surgical?
- What is the expected recovery timeline?
- What are the risks and benefits of MPFL surgery?
- Will I need additional procedures, such as tibial tubercle transfer or cartilage repair?
Recovery and Rehabilitation
Immediate Post-Operative Care:
Patients typically go home the same day with the knee in a brace. Weight bearing is allowed as tolerated, but the brace keeps the leg straight while walking for 4–6 weeks.
Pain Management:
A local anesthetic block is often used during surgery, followed by oral pain medications as needed.
Physical Therapy:
- Begins within the first two weeks
- Focuses on restoring range of motion, strength, and function
- Gradual progression to advanced exercises and sports-specific training
MPFL Surgery Recovery Timeline:
- Most patients return to full activities and sports between 4–7 months after MPFL surgery, depending on individual healing and rehabilitation progress and the specific sport that they participate in..
Tips for Success:
- Adhere to physical therapy protocols
- Communicate any concerns with your surgeon or physical therapist
- Be patient—full recovery can take several months. Initially, it may be somewhat painful, but don’t let that deter you from getting the surgery you need to return to an active lifestyle.
Difference Between MPFL Repair vs. Reconstruction
Feature |
MPFL Repair |
MPFL Reconstruction |
Indication |
Rare as failure rate is much higher | Complete or chronic tears, recurrent instability, first time dislocators with multiple risk factors for recurrence |
Technique |
Suturing the native ligament | Using a graft (autograft or allograft) to recreate the ligament |
Outcomes |
More likely to lead to stiffness and higher failure rate | Shown to have lower redislocation rates and better function |
Preferred For |
Acute, isolated injuries | Most cases of recurrent or chronic instability |
Patient Success Stories
Patients often report dramatic improvements in stability and quality of life following MPFL reconstruction. Watch video testimonials from individuals who have returned to the sports and activities they love after MPFL surgery, highlighting the benefits of the procedure.
Frequently Asked Questions (FAQs)
How do I shower after MPFL surgery?
Cover the surgical site with a waterproof dressing. Avoid submerging the knee until the incision is fully healed.
How painful is MPFL surgery?
Expect some pain, especially in the first week; it will improve steadily as you heal. Local anesthetic blocks and medications help manage discomfort initially.
Is knee popping or cracking normal after surgery?
Some popping or cracking can occur as the knee heals and regains motion. Discuss persistent or ongoing pain symptoms with your surgeon.
When can I walk or drive?
Walking with a brace is allowed immediately, but driving is only safe once you can control the leg comfortably—usually after several weeks, depending on which knee was operated on and your recovery progress.
Is numbness normal?
Some numbness around the incision is common and often improves over time.
For additional answers to questions I’ve received about knee injuries and treatments, please check out my FAQs and Patient Information pages.
Medial Patellofemoral Ligament Reconstruction Surgery
When non-operative measures are unsuccessful or not a viable option, MPFL reconstruction surgery is a highly effective knee ligament surgery for those suffering from patellar instability. With proper diagnosis, a skilled surgeon, and dedicated rehabilitation, patients can expect excellent outcomes and a return to the activities they love.
Please reach out to my office if you want to discuss your MPFL reconstruction options or get a second opinion.
The MPFL image file is licensed under the Creative Commons Attribution 4.0 Unported license.