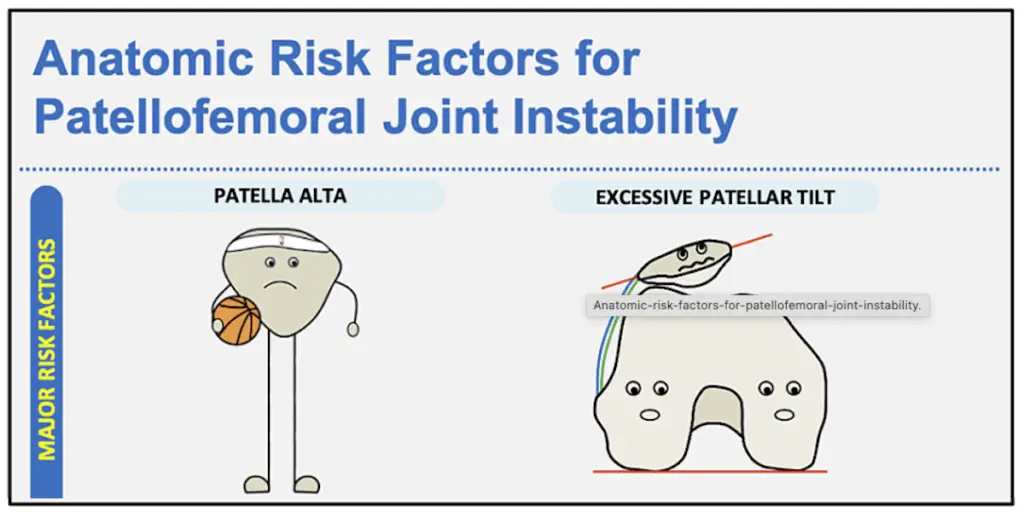
Recently, I came across this excellent infographic and description of anatomic risk factors for patellofemoral joint instability in Cureus.
I spend all day drawing pictures for patients and explaining the risk factors for patellar instability. It’s complicated, that’s for sure! When it comes to sorting out which surgery is required for patellar instability, it comes down to how significant a patient’s anatomic pathology is and what is easily modifiable. Here are a few things to keep in mind:
1. The MPFL is always torn or stretched after a patellar dislocation, so if a patient requires surgery then we reconstruct the MPFL.
2. For patients with elevated TTTG or lateralized tibial tubercles, we consider a tibial tubercle osteotomy to realign the extensor mechanism.
3. Many of these patients suffer from patella alta, which increases the contact stress on the inferior patella and proximal fat pad. This also may lead to patellar instability as the patients must flex their knee more in order to engage the patella in the trochlear groove. In these patients, we may need to distalize or move the patellar tendon attachment more distal in order to change the contact forces or increase the arc of motion in which the patella sits in the trochlear grove.
4. Some patients suffer from severe trochlear dysplasia in which the front of their knee has significant pathology or malformation of the bone. Occasionally, these patient may benefit from trocheoplasty to reshape the groove, which is a difficult surgery fraught with complications. It ultimately results in a “square peg in a round hole” as one doesn’t reshape the patella. This is a complicated issue and it takes a lot of thought to sort out these problems.
Take a look at the article and accompanying infographic to get more detail: Anatomic Risk Factors for Patellofemoral Joint Instability: An Infographic as a Visual Learning Tool.
The header image is a clip of the full infographic to give you an idea of what it looks like, but you really should check out the full image.