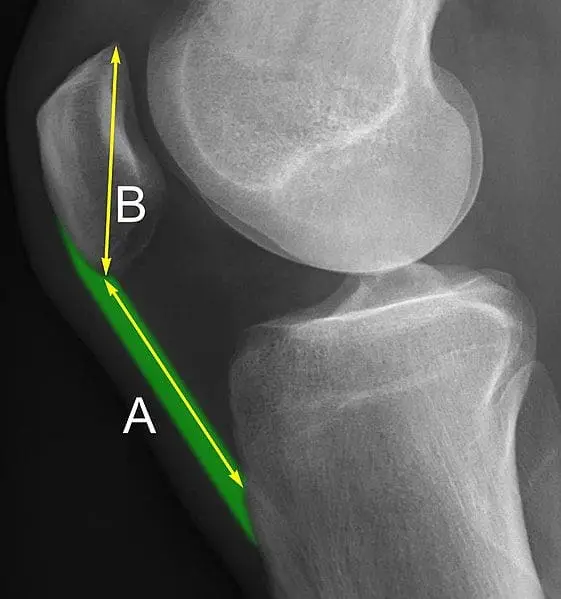
Patella baja is characterized by a loss of patellar height and can develop as either an acute or chronic complication following a knee injury or surgical procedure. The purpose of this review is to describe the diagnosis and management of patella baja and highlight the senior author’s surgical technique.
Recent Findings
The pathogenesis of patella baja involves a complex interaction between quadriceps dysfunction, immobilization, and inflammation leading to infrapatellar scarring and adhesions. It is associated with fractures about the knee and can result as a complication of surgical procedures such as anterior cruciate ligament (ACL) reconstruction, particularly bone-patellar tedon-bone autografts, high tibial osteotomies (HTOs), tibial tubercle osteotomies (TTOs), and total knee arthroplasties (TKAs). Patients with patella baja can have limited knee range of motion, anterior knee pain, significant weakness with active knee extension, and an extensor lag. Surgical intervention is indicated in cases of symptomatic patella baja. Treatment strategies include tibial tubercle proximalization, patellar tendon lengthening, and patellar tendon reconstruction. Allografts and autografts can be utilized to augment tendon lengthening or reconstructive procedures. Various small case series have reported favorable outcomes for these procedures.
Read more in Current Reviews in Musculoskeletal Medicine.