This article discussed outcomes of patellofemoral arthroplasty, which is one type of partial knee replacement. When I first started doing this type of surgery it was very rare. I had never seen one done in residency or fellowship.
The reason I became interested in it was that a new generation of implants had been introduced. The old implants required a lot of freehand cutting (not very reproducible), a short implant so some patients would feel their kneecap slip off the implant, and a higher complication rate. The new implants, however, aimed to make the surgery more reliable with implants that better reproduced the patient’s own anatomy.
I found this study lacking in that they only had 45 patients (and this included several surgeons over several years). I do more than fifty of these surgeries a year and therefore when I look at my results, I think that I can draw more concrete observations.
Over the years, I have learned a lot about how to optimize this surgery. For example, I rarely do a standard medial approach, because most of these patients are lateral patellar trackers and benefit from a lateral lengthening approach (rather than a lateral release).
Furthermore, I typically get a MRI on all patients to make sure that I can see early arthritis in their medial or lateral compartment. I do that so I can (hopefully) minimize the risk of revision to total knee arthroplasty after patellofemoral replacement due to progressive knee arthritis.
There is no perfect operation, but for many patients with patellofemoral arthritis, I think patellofemoral arthroplasty is a pretty good option.
Read the original Cureus article: “Functional Outcomes, Survival Rate, and Complications of Patellofemoral Arthroplasty: Mid-Term Results From Independent Center.“
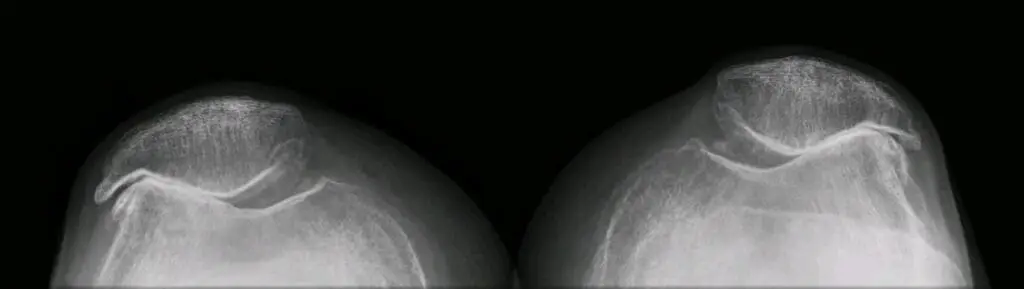
Image source: X-ray of severe patellofemoral osteoarthritis via https://commons.wikimedia.org/wiki/File:Patellofemoral_Osteoarthritis_Severe.jpg
<https://creativecommons.org/licenses/by-sa/3.0>, via Wikimedia Commons